During your pregnancy, you may have noticed that your baby is being unusually quiet and calm.
While normally this would be a good sign, when the baby is still in the womb, it’s more likely that you have a baby in distress.
A baby in distress, more commonly known as fetal distress, is a term used to describe a state of the fetus that’s suffering from a lack of oxygen, among other, less common issues. It can happen during labor and pregnancy.
It’s a condition that’s somewhat tough to recognize, but one mothers should always be aware of.
While a rather common occurrence as fetal distress is bound to occur at some point during every fourth pregnancy, give or take, it’s not something to be taken lightly as any potential consequences are serious and can prove crippling for both mother and baby.
Now, I’m not trying to frighten you, just pull your attention toward a rather serious issue that you should keep an eye out for.
I know first hand how panic-inducing a pregnancy can be, especially for someone who’s going through it for the first time.
But don’t lose hope. While a serious issue, it doesn’t mean that it will immediately lead to the worst-case scenario.
With a good amount of devoted attention to notice the early signs of fetal distress and a quick enough reaction, you’ll be able to prevent any of the potential problems and complications from becoming permanent.
Signs Of Fetal Distress
Luckily, there are many telltale signs that you should be aware of regardless if they’re considered a common occurrence during pregnancy or not.
1. Lack of fetal movement within the womb

While not a factor during early pregnancy since the baby hasn’t developed enough yet, it becomes a key indicator of any problems occurring within the womb.
Once your baby grows large enough to start kicking every so often, you’ll start feeling that ever-present joy of pregnancy that every mother talks about, especially because your brain is reassured that everything is okay with the baby.
This is a sign that good fetal health is being maintained.
The moment you feel a change to the rhythm or the lack of the baby’s movement altogether, despite being well into your second trimester, it’s a cause for concern.
It might be that your unborn baby is in fetal distress and that there’s something wrong with their oxygen supply.
Their blood flow might be obstructed, causing the aforementioned oxygen deprivation, which poses great risk for their well-being.
The moment you feel like something is off, you shouldn’t hesitate to call your midwife or family doctor for a check-up.
No sign should ever be disregarded regardless of how meaningless it might be because, as I’ve said before, the risk of the issue being something major is overwhelming.
Better to be safe than sorry.
2. Stronger cramping

It’s not even the number; it’s the strength of a cramp and you should definitely go to see your doctor for a diagnosis if they become a lot more severe and frequent than before.
If you keep getting painful cramps only during urination and it’s causing you an unusual amount of pain, it might be a sign of a urinary tract infection (UTI) and should be relayed to your doctor immediately so you don’t risk it endangering you or your baby.
Preterm labor is also a known cause of cramping which may result in a premature delivery, cutting your child off from the precious nutrients she was feeding off of too early, which tends to lead to having a baby in distress and the need for an incubator.
On the other hand, if your cramps are occurring in the upper abdominal area and causing you an immeasurable amount of pain, it might be a sign of pre-eclampsia.
Pre-eclampsia is a condition that shouldn’t be taken lightly as it can develop potentially life-threatening complications for both you and the baby – from seizures to high blood pressure and even liver failure in the mother’s case, to issues with proper blood flow to the placenta, leaving the fetus with a lot less food and not enough oxygen, resulting in the delivery of an underdeveloped baby with low birth weight.
If you suffer from a lot of stress or naturally high blood pressure and you notice protein in your urine (a foam that doesn’t seem to go away even after a flush or white residue inside the urine itself) get a check-up done as soon as possible.
These are all telltale signs of pre-eclampsia and if you manage to detect them early enough, you’ll be able to avoid any severe problems and life-long complications for either you or your darling child, as long as you follow what your doctor tells you to do.
If your cramping is followed up by vaginal bleeding, then you might be at risk of a miscarriage.
This is the most severe case and you should dial your doctor’s phone number immediately because the faster they can react, the higher the chances of preventing such a dreadful scenario.
While some bleeding, also known as vaginal spotting, is normal during pregnancy and indicates that everything is going smoothly (especially if the bleeding is pinkish), the moment you see it change color to a browner tone or a completely black, know that it should be a cause for concern.
3. An overabundance or lack of amniotic fluid

Polyhydramnios or high amniotic fluid levels can lead to several complications mentioned above.
They range from bothersome, like maternal breathing difficulties and unusual positioning of the baby inside the womb, to some rather serious and life-threatening ones like umbilical cord prolapse and postpartum internal bleeding (hemorrhaging).
Meanwhile, in case of low amniotic fluid levels or oligohydramnios, the issues can be quite dreadful, accounting for several birth injuries on top of everything else.
The most common ones are intrauterine growth restriction, compression of the umbilical cord, or meconium aspiration, which is something that we’ll get to next.
There’s even a greater risk of miscarriage if it’s not treated as soon as possible, so please don’t take the warning signs for granted.
If either are left untreated, they can develop into life-crippling problems for your child like HIE (hypoxic-ischemic encephalopathy) and even cerebral palsy.
Should you notice your amniotic fluid leaking out, immediately contact a medical professional and schedule an emergency appointment to take a look at what the issue might be and assess it properly.
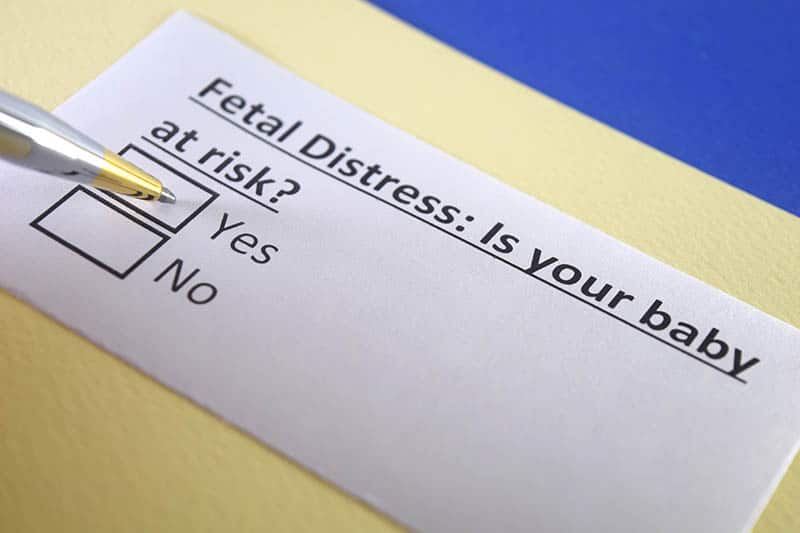
4. Abnormally low fetal heart rate
The doctor or the midwife might keep you in the hospital for a bit to observe the baby’s heart rate utilizing EFM (electronic fetal monitoring) until they discover the cause of fetal distress.
If it continues being low, it will start causing worse problems for the child, this is why all healthcare professionals are urged to not tarry when it comes to any issues involving babies or pregnant women and why they have priority to begin with.
Minutes waiting could be the difference between losing a life and saving one (maybe even two).
5. Abnormally high or low maternal weight gain

Should you deviate from the norm, it may cause a number of different problems, depending on which end you ended up crossing.
The main problem with gaining very low amounts of maternal weight means that your baby might not be getting enough nutrients and oxygen as a consequence, leaving the baby in distress and severely underdeveloped.
This is called intrauterine growth restriction (IUGR).
The sooner you notice this problem and call it in with your doctor, the lesser the consequences will be and the more chance you’ll have on remedying the issue before it develops into something worse (placental abruption or preterm labor).
On the other hand, gaining excessive amounts of maternal weight isn’t good for you or the baby either.
For the mother, it can lead to increased chances of gestational diabetes, while your child can have a different issue: macrosomia.
Macrosomia is a condition where the baby is unusually large for the developmental period and, if it happens, needs to be discovered as soon as possible and reported to your doctor or physician so they can know how to proceed further.
That’s because it’s a rather delicate situation and if you start going into labor and the doctor tries going through with a natural birth, the baby might get stuck.
This is going to be either due to cephalopelvic disproportion (CPD) where your pelvis is simply too small to let the baby through, or shoulder dystocia where your baby’s shoulder simply gets stuck on your pelvic bone and cannot get out.
While there are ways of getting the baby out through vaginal birth with the use of vacuum extractors, oxytocin substitutes, and forceps, they are prone to causing even more problems (some of them even resulting in permanent brain damage).
The solution for delivery when macrosomia comes into the equation is to go through a cesarean section. There simply is no way around it because the risk is otherwise too great for a vaginal birth.
Causes Of Fetal Distress

Some of these have been touched upon earlier in the article, but they definitely need their own individual spot.
1. Shoulder dystocia and vacuum extractor method
What causes fetal distress in this case are the methods utilized to get the baby out because whether the forceps is used, the vacuum extraction method, or Pitocin, your baby’s oxygen will get cut off and they are at risk of sustaining permanent brain damage.
2. An abnormal fetal position

Imagine it like trying to match a square piece to a triangular hole on a baby toy, it’s near impossible unless forced. An abnormal fetal position usually ends in a C-section.
3. A nuchal cord
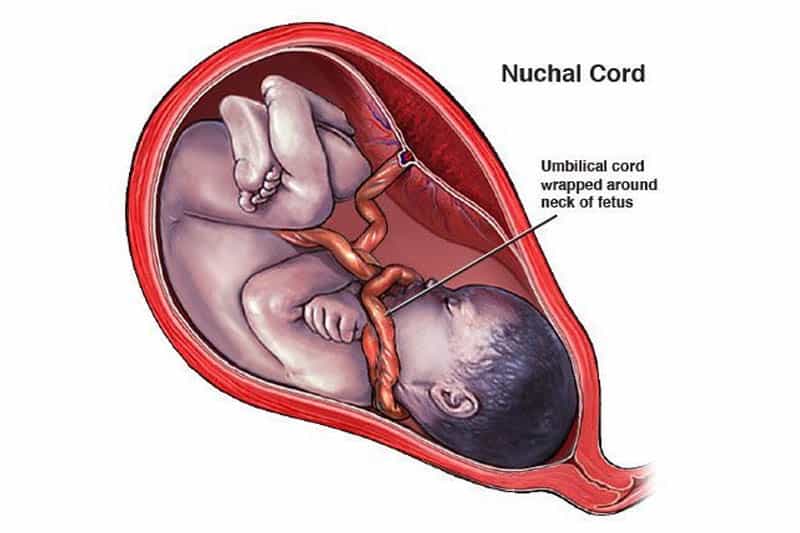
It’s not a pretty picture to see or even hear about, but it does happen and is a great source of distress due to oxygen deprivation and the sense of being choked.
4. Placental abruption
Sounds similar to pre-eclampsia, doesn’t it?
Well, that’s because preeclampsia is one of the potential factors that increase the risk of placental abruption in the first place, followed alongside rather severe and persistent cramps.
Thankfully, it’s a very rare condition that only happens in about 1% of all pregnancies, though should still be taken into account.
The abruption can be either partial or total.
In case of a partial abruption, your pregnancy can still continue in a somewhat regular manner with a lot of monitoring and potential hospital stay just in case.
On the other hand, a total placental abruption is always going to end in an induced delivery because it is the safest option for both the mother and the baby in question, despite not being the most desirable, depending on how far along your pregnancy is.
Based on the severity, a C-section might be required as well, but at that point, that’s the least of your worries.
5. Meconium aspiration
You see, meconium is a sort of prenatal poop that forms inside of the baby’s digestive tract as he develops in your womb.
Normally, it’s not ejected out of his system until after delivery has been completed, but should the baby be affected poorly in any sort of way, he can eject it even while still in utero.
This causes a potential risk of them ingesting it alongside the amniotic fluid near the designated birth period, which can develop dangerous complications like HIE, pneumonia, PPHN (persistent pulmonary hypertension) or, in the worst-case scenario, lung collapse.
When your water breaks, check your maternity pad for any specs or stains of brownish black. If there are any, chances are high that it’s meconium on the pad and that meconium aspiration might be an issue you’ll be having to deal with prior to delivery if possible.
Treating Fetal Distress: Why Early Detection Is Important

If you do, the doctors will be able to react early enough where they won’t have to resort to any drastic measures and will be able to prescribe you the right steps that you can take to lower the chances of any of these situations happening in the future.
Each and every case requires specific treatment, so only trust what your doctors say rather than relying on the internet for help with such a serious issue.
Even a simple change in positions (sleeping on your left side) could help alleviate the risk somewhat. A lot of pillows or a nice, large pregnancy pillow can help make that position a lot more comfortable and prevent any movement during sleep.
The sad part is that there isn’t really much else you can do to completely prevent these cases of fetal distress from happening, apart from keeping a close eye on what your precious baby is doing inside your tummy.
And, of course, doctors and any other medical staff that are assisting you need to devote their full attention to it because any mistake and misjudgment can be devastating, even leading to them losing their license and being accused of medical malpractice.
That’s why, when they see that the C-section is the only way for the baby to be saved, they’ll do it ASAP.
The Difference Between Fetal Distress And Birth Asphyxia

But, fetal distress is a much broader term than just that since it encompasses any issues the fetus may have during the pregnancy period.
Due to the aforementioned confusion caused between the two, the ACOG (American Congress of Obstetricians and Gynecologists) is pushing to remove the term birth asphyxia entirely and that the term fetal distress be renamed to NRFS (nonreassuring fetal status.)
This is mostly due to the inappropriate use of the terms mentioned, which tend to often cause a lot of confusion in medical reports.
They’re also looking to add the other causes of fetal distress under that tag that have been found out more recently, like having a low biophysical profile, the existence of fetal tachycardia and bradycardia, as well as both late and repetitive fetal heart rate decelerations.
While this has been proposed, the term fetal distress is still widely used and is yet to be replaced mostly due to habit.
Final Words
While having a baby in distress is something you cannot influence greatly outside of trying to live a healthier life for that slight chance reduction, you shouldn’t stress about it too much either. That part is outside of your hands.
Try focusing on the good future you have planned with your upcoming child and trust your doctors to make the best decisions.
They do have your best interests in mind, as do any other healthcare professionals.
Listen to their advice and pay attention to the way your growing bundle of joy is acting, and you should do just fine.
References:
Committee on Obstetric Practice. (2005). ACOG Committee Opinion. Number 326, December 2005. “Inappropriate use of the terms fetal distress and birth asphyxia. Obstetrics and gynecology,” 106(6), 1469.
Like this post? Please share or pin it for later. You can also stay in the loop and follow us on Facebook, Instagram or Pinterest.
This post contains affiliate links. Please see our full disclosure for more info.